The transition from hospital to post-acute care can be challenging for patients and their caregivers, especially in instances where they lack a proper support framework. According to the NHS, the highest proportion of emergency readmissions occur within 30 days of the most recent discharge, at an estimated 15.5% between 2021/2022. Out of these events causing readmission, 61% have been found to be preventable.
Late last year, it was reported that about 14,000 hospitalised patients across England were unable to be discharged due to a severe shortage of social care. The situation was particularly dire in the South-West, where over 20% of patients were medically fit to leave but remained stuck in hospital due to a lack of available care options. This caused bed occupancy rates to soar to 44% higher than pre-Covid levels, placing a significant burden on hospitals that were already stretched thin. As a result, hospitals struggled to manage both these patients and new admissions, which were also at a record high.
This surge in patients highlighted the importance of hospitals being equipped to handle discharges enmasse. To relieve hospitals of the challenges of providing in-house post-acute care, home-based and palliative providers must be empowered with the skills and technology needed to cater to patients post-discharge. This will ensure that the benefits accrued across the health continuum are not reversed during the transition, and that healthcare providers proactively engage their patients, create meaningful connections and effectively help guide successful outcomes.
With burgeoning health information technology, such as Electronic Health Records (EHRs), data integration and artificial intelligence, hospitals can now provide integrated patient care management regardless of time and place. These tools can help lower the rate of hospitalisation, improve experiences for those who have been discharged, and aid providers in handling their patient load while optimising the management of their resources.
Managing Transitions in Hospitals with Technology
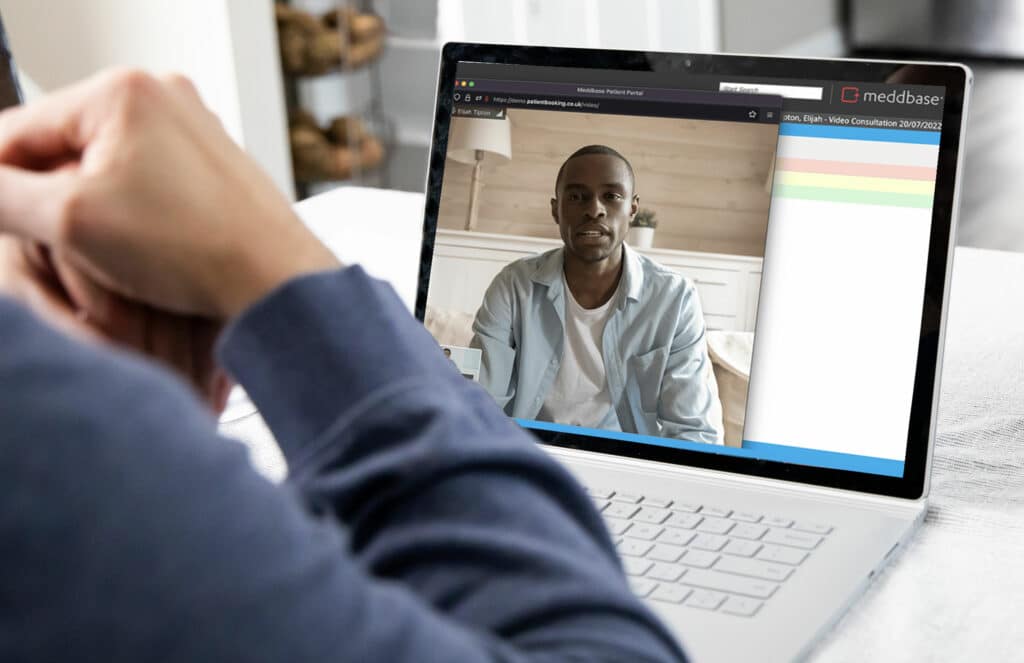
With the integration of robust data into telehealth systems, caregivers can access patient insights, trends and a wide array of patient information on-demand. This ability to collect, analyse, and present data plays a crucial role in managing the care of patients and informing resource allocation decisions in hospitals. This information also helps caregivers to make enlightened decisions about the most appropriate care setting for a patient and the optimal timing for transition to the setting. With this comprehensive view of a patient’s journey, clinicians can easily place patients in environments that are most likely to fast-track their recovery.
The use of clinical decision support tools can also guide care transitions by converting data into practical and easy-to-understand insights. Because clinicians can access records regardless of their location, it is possible for them to quickly recognize health trends and identify patients who are ready to be transferred to another care setting or transition out of the hospital. This approach offers complete oversight throughout the entire process.
Since 2010, hospitals in the UK are no longer paid for costs of readmissions occurring within the first 30 days of discharge. If physicians don’t take enough caution to ensure that patients and their caregivers are equipped to handle the transition from the hospital, they bear the brunt should readmission occur. It is therefore imperative that every hospital has an air-tight strategy to prevent transitions in the wrong direction.
At Meddbase, we provide solutions that enable continuous data capture, advanced visualisation, and predictive analytics that empower clinicians to deliver proactive care and guide timely interventions, greatly improving patient outcomes.
Streamlining Out-of-Hospital Transitions
Among the major problems that hinder smooth transitions from hospitals to post-acute care, the one that has been cited most is the retared flow of patient information across practices. According to this source, up to a third of receiving caregivers don’t have access to patient records and test results from hospitals and only 12 to 34 percent of discharge summaries reach after care teams.
Since healthcare is now siloed, with patients having more than one specialist at a time, it is easy for crucial information to fall through the cracks as the patient moves along the healthcare pipeline. For instance, in one study conducted over a period of 18 months on 1000 patients, 37% were readmitted on the grounds of adverse drug reactions (ADRs), which were found to be, for the most part, preventable. Without proper medical reconciliation (the process of compiling all the medications a patient is taking, including medication names, dosages or strengths, frequencies of use, and routes of administration), the risks of ADRs are exponential. If the receiving carer does not have sufficient knowledge of the drugs their patient is on, they are bound to have difficulties with adherence and overuse, or may even recommend counteractive drugs.
Before moving your patient to a palliative care facility, it is therefore essential that you compile their information into a comprehensive report that can be passed on to their subsequent caregivers. And because it can be time-consuming, dealing with bulky and dynamic data, it is advisable to make the switch to EHRs if you haven’t yet. Meddbase‘s EHR provides a centralised, interoperable platform that fosters the smooth flow of information across practices. With its easy-to-operate interface, all caregivers can instantly access summarised or in-depth patient information on the go. This ensures that before admission, receiving facilities can assess the patient’s history to confirm that they have the right staff to care for them based on their respective healthcare requirements.
Integration with Remote Monitoring Technology
A key part of ensuring seamless out-of-hospital transitions is to look out for early signs of deterioration, so that timely interventions can be implemented before they escalate. At present, most physicians monitor their patients through regular in-person follow-ups, which can be difficult to coordinate especially if regular monitoring is required or if the patient is immobile. Switching to remote monitoring however, can bring about significant cost savings without compromising patient outcomes.
Wearable technologies have become increasingly popular and can play a vital role in the transition of patients from hospitals to their homes. In recent years, these technologies have become increasingly complex, allowing for the testing of a myriad of parameters. Now, wearables can track and record an array of biometric data, such as oxygen levels, blood pressure, glucose levels, sleep patterns, and even mental health indicators. Some fitness watches even have built-in electrocardiogram (ECG) capabilities. By monitoring real-time vital signs provided by wearable technologies, healthcare givers can track the progress of their patients without the need for in-person appointments.
Patient non-compliance has proved to be a thorn in the sides of pharmaceutical companies and healthcare providers. It is estimated that drug non-compliance causes up to 100,000 preventable deaths per year. But with platforms that digitise drug specialty management, abandonment and nonadherence rates have been seen to plummet. Seamless coordination between inpatient, outpatient and home-based care teams using such platforms can help to manage prescriptions and ensure sufficient followup is done on the patients.
In cases where the patient or caretaker assumes full responsibility for all post acute patient care without an adequate understanding of post-discharge instructions, more than 30% are likely to wind up back in the hospital less than 6 months after discharge. This is why physicians should ensure that patient literacy levels are high as they administer care, this way, when patients are at home they can handle their treatment adequately. After discharge, hospitals should ensure that patients and caregivers can access patient portals that should, on top of their exhaustive medical records, include informational materials to enhance patient education. Simple interventions like leaflets to explain diagnostic information have been shown to increase patient understanding of their diagnosis from 77% to 100%, and medication literacy from 27% to 71%. The portal provides a forum for patients to track their progress, keep in touch with their practitioner, manage appointments and payments.
At the end of the day, these technologies allow for the most important member of the team—the patient—to have more agency over their treatment as they transition away from hospitals.