Meddbase’s pilot study with NHS Humber and North Yorkshire ICB on using technology to improve Diabetes prevention referrals has been featured in Building Better Healthcare. Read the full article on Buildingbetterhealthcare.com.
Texts prompt increase in referrals to NHS diabetes programme
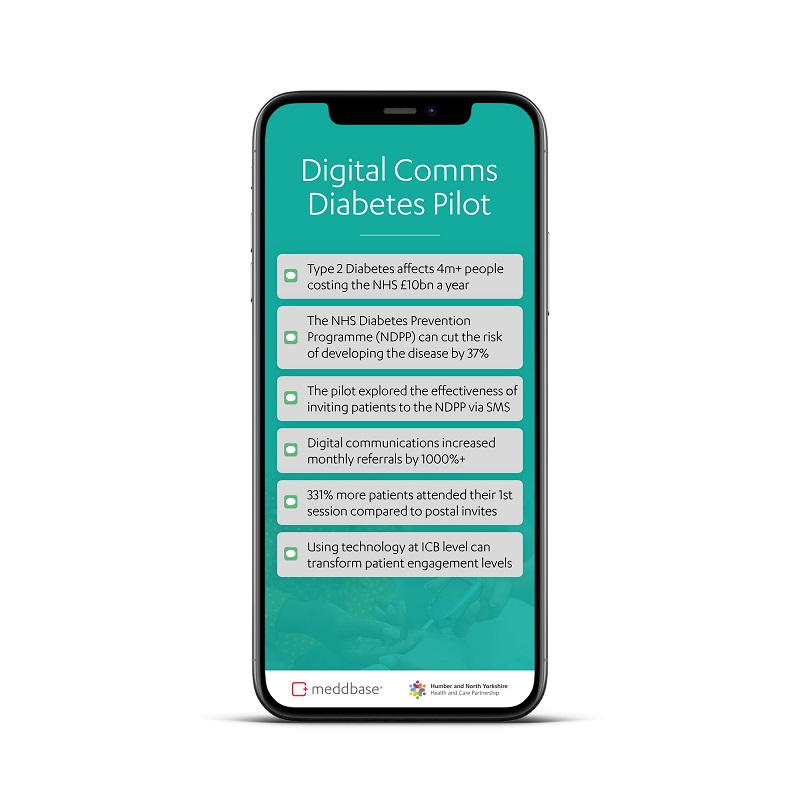
A pilot study of 795 pre-diabetic patients has shown the significant potential of text messaging to engage patients with health intervention programmes.
The study was designed to explore whether using the latest digital communications software, and managing it at an Integrated Care Board (ICB) level, is more effective than traditional postal invites when it comes to engaging patients in healthy lifestyle programmes.
Conducted by NHS Humber and North Yorkshire Integrated Care Board, with support from its clinical technology partner, Meddbase; the pilot led to an increase in referrals to the NHS Diabetes Prevention Programme (NDPP) of more than 1,000%.
It found that using patient identification tools and automated text message prompts led to:
- A 1,000%-plus increase in NDPP referrals – from an average of 32 referrals per month to 363 per month
- A 331% increase in the number of patients attending at least one session of the NDPP programme (defined as ‘Milestone 1’) – with the previous monthly average of 16 patients rising to 69 in the first month of the study
- A 181% increase in the number of patients attending sessions over a three-month period; with the findings showing an average of 45 patients reaching Milestone 1 each month, compared with the pre-study baseline average of 16
The results from the study and the key learnings for ICBs, including the importance of data quality and the need to facilitate patient choice, are explored in detail in a new white paper report entitled It’s your GP texting: Utilising technology at ICB level to deliver a tenfold increase in referrals to the NHS Diabetes Prevention Programme.
Patient engagement
And the findings demonstrate how utilising technology at ICB level has the potential to deliver huge increases in patient engagement in healthy lifestyle programmes, such as the NDPP.
The NDPP was developed by NHS England and Diabetes UK and offers patients at risk of type 2 diabetes free support from an evidence-based lifestyle programme.
Some two million people in the UK are classed as having pre-diabetes, meaning they are likely to develop the condition if they do not change their lifestyle.
To date, one million people have followed the programme, with data showing that it reduces the chances of developing diabetes by 37%, but can only have the desired impact with patient participation.
The study was conducted using software from Meddbase, an advanced clinical management provider.
 The Meddbase system enables ICBs to identify eligible patients and schedule text prompts
The Meddbase system enables ICBs to identify eligible patients and schedule text prompts
Capturing information
The technology was used to enable the ICB’s engagement officer to quickly identify eligible patients, check them against criteria, and then schedule text message prompts, while also capturing information to update Electronic Patient Records.
Commenting on the pilot, Scott Walker, senior partnership officer for diabetes at NHS Humber and North Yorkshire ICB, said: “We’ve seen phenomenal success with this pilot, which was driven by user need.
“Previously, we had to wait to achieve the critical mass required to make our diabetes prevention programme viable, but we can now confidently say we will have enough patients to start a group.
“In fact, the success of the pilot has given us the confidence to bring in additional human resources to manage patient conversions. That’s the beauty of this solution – the untapped potential is huge.”
A huge impact
Dr Tom Milligan, a GP and the clinical lead for diabetes in Humber and North Yorkshire, added: “Before this study, I thought we were doing NDPP referrals well. But, in fact, we were missing hundreds of patients with pre-diabetes.
“The software used for this pilot enabled the ICB to conduct advanced searches for the first time, so we could identify, invite, and refer patients who would otherwise have been missed.
“The result was far greater uptake of the NDPP as well as significant time saved for clinical staff.
“Given the current capacity challenges within General Practice, and the cost to the NHS of lifestyle-related conditions like type 2 diabetes, the findings here could have a huge impact.”